What is Pelvic Fascia? The Missing Piece in Women’s Health
If you’ve been doing pelvic floor exercises, squeezing when you’re told to squeeze, and still feeling like your core isn’t fully coming back online… this may be the missing piece. Maybe the leaking persists. Maybe the heaviness hasn’t lifted. Maybe intimacy feels different. Maybe your abdomen still feels disconnected no matter how strong you try to make it.
For decades, women’s health has centered primarily on muscle. Strengthen the pelvic floor. Tighten the core. Brace better. Engage more. And while muscle strength matters, there’s a deeper layer involved in every pelvic health condition women experience.
That layer is fascia. And it may be the most overlooked aspect of women’s health.
Let’s take a closer look at why pelvic fascia plays such a central role in healing conditions like diastasis recti, prolapse, bladder leaks, chronic pelvic tension, and the core dysfunction so many women experience, especially after pregnancy.
What Exactly is Fascia?
For many years, fascia was described simply as “connective tissue.” But that definition doesn’t capture its true role in the body.
Western medicine is only just beginning to acknowledge fascia for what it really is: a living, responsive crystalline matrix that surrounds and integrates your muscles, organs, bones, vessels and nerves into one continuous system. It provides structural support and also plays a critical role in communication, coordination, and pressure regulation.
Fascia is fluid and adaptive. Some researchers describe it as having liquid crystalline properties, meaning it can transmit and reflect light and mechanical information in sophisticated ways. While research is still evolving, what we do know is that fascia is highly responsive to stress, breath patterns, posture, and lived experience.
It is not passive tissue. It is constantly adapting to how you live.
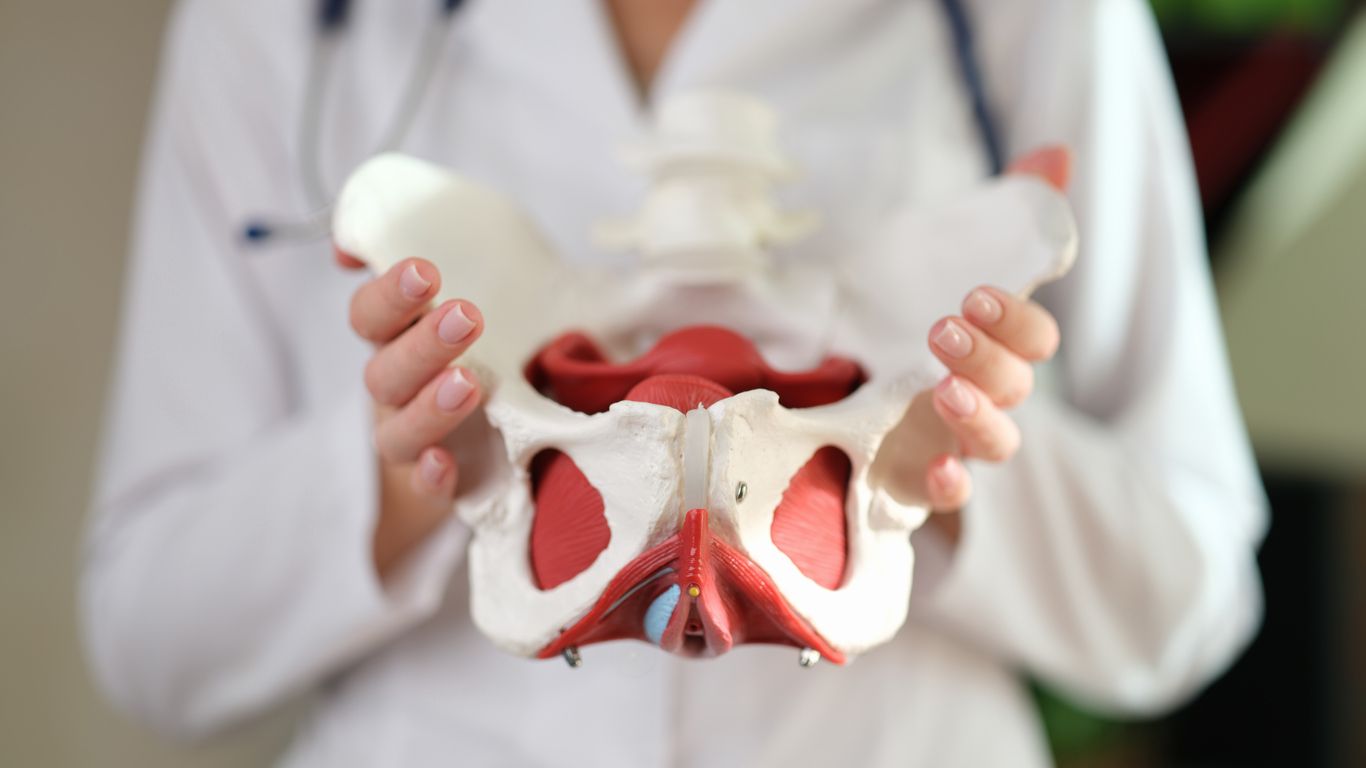
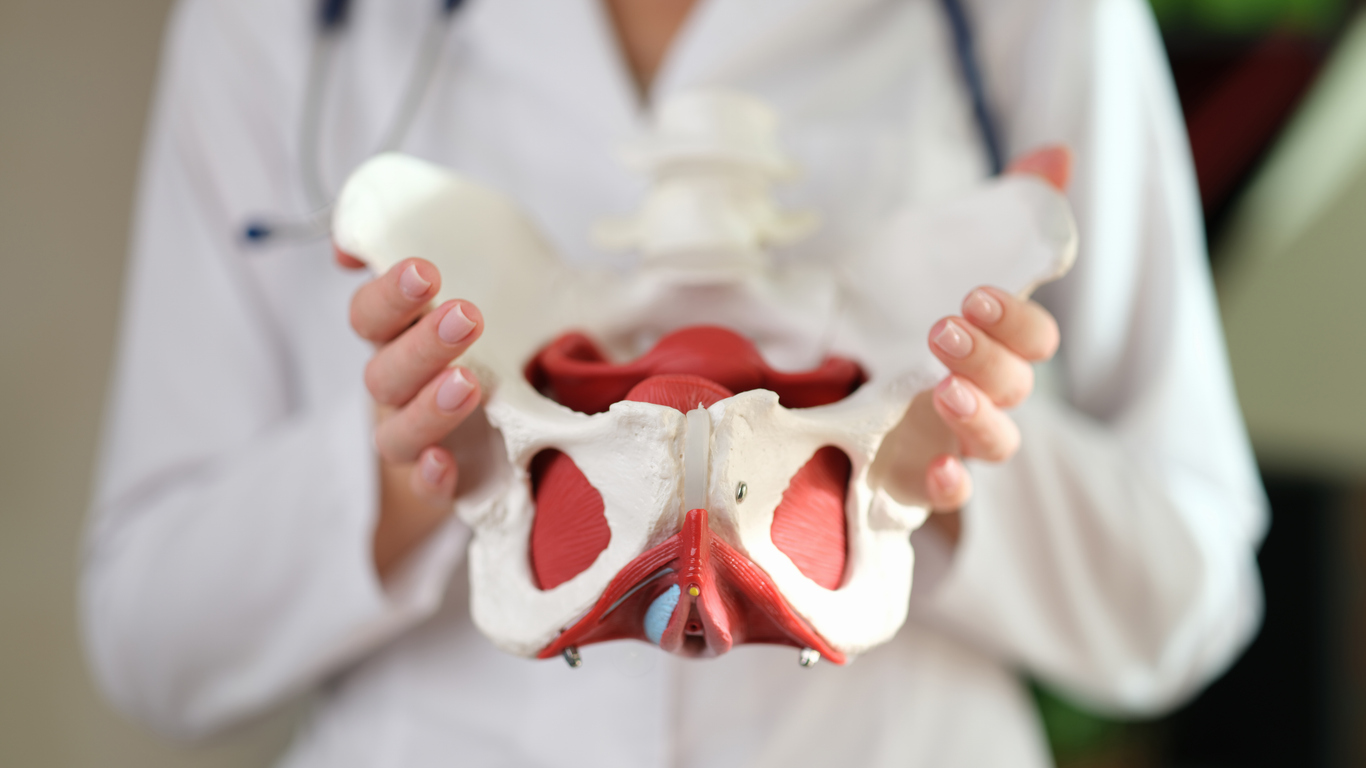
Why Pelvic Fascia Matters for Women at Every Life Stage
There are three properties of fascia that make it especially important in women’s health.
First, fascia transmits information. It forms one continuous web throughout the body. Tension in your ribcage can influence your pelvic floor. Scar tissue from abdominal surgery can affect bladder function. Chronic jaw clenching can increase pelvic tension. When we isolate strengthening without considering this interconnected system, we often miss the bigger picture.
Second, fascia receives information. It responds to emotional stress, breath holding, physical load, and hormonal changes. During pregnancy, birth, perimenopause, times of high stress, or intense athletic training, pressure dynamics in the body shift dramatically. If your nervous system perceives instability or threat, fascia adapts by tightening and bracing to protect you. Over time, that protective pattern can lead to chronic dysfunction.
Third, fascia stores adaptive patterns. Your body reorganizes around every experience you move through — pregnancy, birth, trauma, surgery, chronic stress, even repetitive posture at a desk. These adaptations are intelligent, but they can create long-term tension and imbalance if not reorganized.
That’s why healing is rarely just about “getting stronger.” It’s about restoring how the entire fascial system manages pressure, tension, and coordination.
The Pattern Nobody Talks About
What are we treating most in women's health? Pelvic floor dysfunction.
What's the pelvic floor made of? 70% fascia.
Diastasis recti is a connective tissue issue involving the linea alba — fascial tissue. Prolapse involves the fascial support system that organizes and suspends the pelvic organs. Bladder control depends on how pressure is distributed and absorbed through the fascial system.
I see these conditions constantly:
- Diastasis recti
- Bladder leaks
- Prolapse
- Pelvic pressure
- Back pain
- Painful intimacy
- Chronic pelvic tension
- Persistent low back or hip pain
- A feeling of heaviness during workouts
- A core that never quite feels stable
And with every single one of these pelvic health issues that I treat in my physical therapy practice, the primary tissue involved is fascia.
Why Traditional Approaches to Pelvic Floor Dysfunction Don’t Work
Most approaches still emphasize voluntary muscle contraction as the primary solution. More Kegels. More bracing. More tightening.
That's not the issue. Muscle engagement is certainly part of the whole system, but the actual tissue we're seeking to change is the pelvic fascia. And fascia doesn’t respond best to force. She responds to pressure, hydration, nervous system input, and integrated movement.
When we ask your waist to narrow, your diastasis to close, your organs to lift, or your bladder to stop leaking, we are asking fascia to remodel. We are asking it to redistribute tension and manage pressure more efficiently.
That's why so many women struggle when they're told to focus on squeezing their pelvic floor through Kegels. It feels like they're working hard, but it's not restoring optimal fascial function.
When fascia is supported properly, pelvic floor muscles begin to function more automatically and efficiently. Strength becomes integrated rather than forced.
Healing Pelvic Floor Dysfunction Begins with Fascia
Inside The Core Recovery Method®, we approach women’s health through the lens of fascial healing because that is the tissue most responsible for lasting change, whether you’re six weeks postpartum, six years postpartum, or navigating a completely different phase of womanhood.
We begin by restoring the system. That means reducing intra-abdominal pressure, decompressing chronically loaded tissues, and helping the nervous system shift out of protective bracing. When the body feels safe and supported, fascia can reorganize.
From there, we reclaim strength. Instead of isolating muscles, we integrate breath, fascia, and functional movement so support becomes automatic. The pelvic floor coordinates reflexively. The abdominal wall responds dynamically. Movement feels stable without rigidity.
Finally, we renew confidence. When pressure is managed well and tissues are functioning optimally, women often notice their waist narrowing, their heaviness lifting, pain resolving, and leaking improving. More importantly, they feel grounded and at home in their bodies again.
When your body learns to release tension and coordinate properly, confidence naturally follows, just like my client Vickie experienced inside The Core Recovery Method®:
“After having three children, I was experiencing pelvic floor dysfunction. I feel stronger and more confident in my body. If you are a woman who has had children, you need this work! You’ll love the results and Angie too. She radiates kindness and is a pleasure to work with.”
-Vickie M.
If you’ve been working tirelessly and still feel like something isn’t clicking, your body is not broken. She’s adapting the best way she knows how.
When we begin working with fascia instead of trying to overpower it, healing unfolds differently. More sustainably. More intelligently. More completely.
You deserve more than symptom management. You deserve restoration at the root.